Anesthesia is a type of medicine that keeps people comfortable and sleeping during a test, procedure or surgery. It can take up to 24 hours to wear off completely. Kids can sometimes feel sick to their stomach or be off balance while recovering. Watch your child carefully until he or she is back to normal.
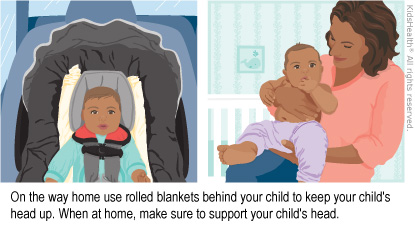
Keep your child's head up:
Be sure to support your child's head. Children may have less head control while the pain or sedation medicines are wearing off.
- Your child should ride in his or her usual car seat.
- To make sure your child's head stays up and to help in case he or she throws up, an adult also should sit in the back.
- If there's no adult in the back seat, try to check often to be sure your child's head has not fallen forward or to the side. If it has, safely pull over and adjust it.
- When your child is resting at home, make sure his or her head is upright.
Offer food and drink slowly:
- Wait to offer your child food or drink until after the car ride home.
- If your child goes back to sleep at home, wake him or her to eat and drink to avoid dehydration.
- Make sure your child is fully awake before offering food or drink.
- Drink: Begin with clear liquids, water, or an electrolyte solution (brand names are Pedialyte® and Enfalyte® and supermarkets and drugstores often have a store brand). Breastfed babies may take breast milk. When your child can drink clear liquids without throwing up, move on to the formula, milk or other liquids your child usually drinks.
- If your child eats solid foods: When your child can drink liquids, next try solid foods. Start with foods that are low in fat and easy to digest, such as toast, crackers, cereal, rice or mashed potatoes.
If your child throws up, follow these steps to avoid dehydration:
- Don't give your child anything to drink for about 1 hour.
- After 1 hour, offer small sips of clear liquid.
- Plain water is not usually best for a child with an upset stomach.
- Never give plain water to your baby under 6 months.
- Electrolyte solution is best. Brand names are Pedialyte® and Enfalyte® (supermarkets and drugstores often have a store brand).
- You also can give frozen electrolyte pops (such as Pedialyte® or a store brand), water ice and flavored gelatin.
- Babies who drink breast milk can still do so.
- Start with 1 teaspoon every 5–10 minutes for 1–2 hours. If your baby is breastfeeding, offer the breast often, but only for about 5 minutes each time so that your baby does not take too much at one time.
- Slowly increase the amount every 15 minutes. If your child throws up again, wait 1 hour, then start over with a smaller amount of liquid.
- If your breastfed baby does not throw up after small amounts of breast milk, you can increase slowly to your usual amount.
- If your child hasn't thrown up after tolerating clear liquid, offer small amounts of plain foods, such as crackers, cereal, rice or mashed potatoes.
- Go back to offering a regular healthy, low-fat diet if your child tolerated plain foods.
- If your child needs to take prescription medicines, give them as directed but only when your child is awake and not throwing up.
Help your child get around safely:
It may take 24 hours to have normal balance and coordination. Until then:
- Don't let your child do anything that requires strength and balance, such as using climbing toys.
- Help your child with standing, crawling and walking.
- Have your child do quiet activities like look at books or play with toys on the floor.
- While carrying or playing with your child, offer extra head support.
Getting back to activities:
- Your child can return to normal activities when fully awake and acting, eating and drinking normally. This is usually after about 24 hours.
- If the health care provider gave you specific activity-related instructions, be sure you follow them, even if your child seems back to normal.

Your child:
- has trouble breathing. Signs are fast breathing and the skin between your child's ribs and neck pulling in tight during breathing.
- is very hard to wake up
Call 911 if you feel your child is having an emergency.