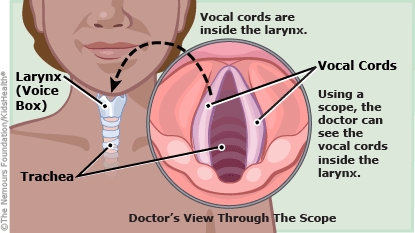
Laryngoscopy (lair-en-GOS-kuh-pee) is a procedure health care providers do to look inside the larynx (voice box), which is below the back of the throat. In direct laryngoscopy, they use an instrument called a laryngoscope (leh-RIN-geh-skope) (or scope, for short) to look directly at the larynx (LAIR-inks).
Your child was under general anesthesia during the procedure. This means your child did not feel the scope and won't remember the procedure.
Your child was watched after the procedure and now can be cared for at home.
Your child may feel tired and have a sore throat, nausea, general muscle aches, or chills for the next day or two. If a biopsy was done, your child may spit out a small amount of blood for the next day. This is normal.

What are the types of laryngoscopes? Two main types of scopes are used for direct laryngoscopy:
- Rigid laryngoscopy: The health care provider uses a firm scope that doesn't bend. It is inserted through the child's mouth into the throat. It lights the inside of the throat and enlarges the view. Usually, it's done while the child is under general anesthesia. The procedure can help a health care provider remove foreign objects or growths, collect tissue samples to examine in a lab, or do laser treatment.
- Flexible laryngoscopy: The health care provider uses a thin flexible tube that can be inserted through the nose or mouth. It has a light and camera on the end, letting the health care provider see the throat through the scope's eyepiece or on a monitor in the room. Usually, it's done in the office or clinic with the child awake, using numbing medicine for the throat. Sometimes it's done while the child is under general anesthesia. The procedure can help a health care provider diagnose problems in the throat and larynx.